Abstract
INTRODUCTION: CD34+ selection has been shown to be a highly effective method to reduce the incidence of acute and chronic graft versus host disease (GVHD) after allogeneic hematopoietic stem cell transplantation (allo-HCT). However it is associated with delayed immune recovery and infections are a major cause of morbidity and mortality. The incidence of Cytomeglalovirus (CMV) reactivation after CD34+ selected allo-HCT has been reported as high as 62-84% in CMV seropositive patients and the incidence of CMV disease was 12.1% (Huang et al, BBMT 2016). CMV and its treatment are known to potentially affect marrow function early post HCT; however data are lacking in patients who reactivate CMV after CD34+ allo-HCT.
AIM: To study the effects of CMV serostatus and CMV reactivation on blood counts recovery in the first year post CD34+ allo-HSCT.
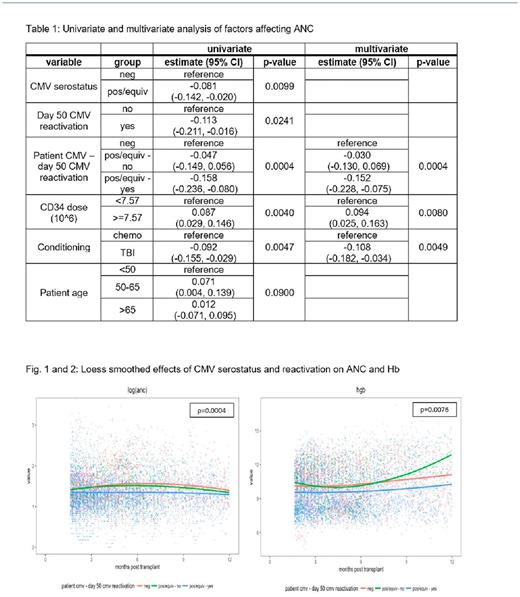
METHODS: CMV viremia was assessed starting on day of engraftment or day 14 post-HCT (whichever occurred first) by quantitative PCR assay if recipient or donor were CMV positive. Per institutional guidelines preemptive treatment with foscarnet, ganciclovir or valganciclovir is recommended when PCR is detected (>137 copies IU/ml). Patients' blood counts data was included from the day of transplant and up to 1 year post-transplant. We studied the effects on counts recovery of patients' CMV serostatus, CMV reactivation by day 50 post HCT, age, conditioning regimen and CD34+ dose. Due to skewness, WBC, ANC, PLT and absolute reticulocyte count values were log transformed. In order to determine the effects of covariates on counts recovery, a mixed effects model with patient specific random intercepts were fit, including both linear and quadratic terms for the time since transplant, as well as each covariate of interest. For all analyses involving CMV reactivation, only counts post day 50 were included.
RESULTS: The analysis included 205 patients who underwent CD34+ allo-HCT between 4/2012-5/2016 for MDS, MPN, AML and ALL. Median age was 55.8 years (range 21.2-73.3). TBI-based conditioning regimen was used in 66 patients (32.1%) and graft source was PBSC in all patients: 178 (87%) from a matched donor; 66 (32%) from a matched related donor (MRD) and 112 (55%) from a matched unrelated donor (MURD) and 27 from mismatched donors (1 related and 26 unrelated donors). Median CD34+ dose was 7.57x106 CD34/kg (0.41-17.52) and median CD3+ dose was 2.1x103 CD3+/kg (0-47.2). CMV serostatus was positive in 119 pts (58%), negative in 77 pts (38%) and equivocal in 9 pts (5%). Ninety-one patients (71% of positive/equivocal pts) had CMV reactivation: median day 27 post HCT (range 14-50). Of the 91 patients who reactivated CMV, 19 (21%) were treated with foscarnet, 26( 28%) with ganciclovir or valganciclovir and 28 (31%) with both agents. 19 (21%) also received CMV CTLs. CMV seropositive/equivocal status was associated with lower ANC in the first year post HCT (p=0.01), but had no effect on Hb and Plt counts. CMV viremia by day 50 correlated with lower absolute reticulocyte count (p=0.03), Hb (p=0.02) and ANC (p=0.02). In univariate analysis, other factors that affected blood counts included CD34+ dose < 7.57 x 10^6 (median) which was associated with lower ANC (p=0.004) and lower Plt count (0.008) and TBI based conditioning which was associated with lower ANC (p=0.005) but higher Plt count (p=0.02). In multivariate analysis, positive/equivocal CMV serostatus, lower CD34+ cell dose and TBI based conditioning, continued to be associated with lower ANC post allo-HCT. Thirteen patients (6%) received a CD34+ selected boost for poor graft function: 10 (8%) in the CMV positive/equivocal group and 3 (4%) in CMV seronegative group (p = 0.378). Despite adversely affecting blood counts recovery post -transplant, CMV serostatus and reactivation had no impact on survival, relapse and non non-relapse mortality.
CONCLUSION: CMV reactivation affects blood counts recovery post CD34 selected allo-HCT. Despite being an early event, its adverse effects on peripheral blood counts persist for months post-transplant. Whether the cytopenia is driven mostly from CMV infection or from CMV directed therapy is unclear. More effective and less myelosuppressive therapies are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal